
CASE OF THE DAY 11 NOV
Question:
Young man with gradual onset neck pain and asymmetrical right upper extremity weakness with normal sensory examination. There was no significant previous history of trauma or any chronic illness.
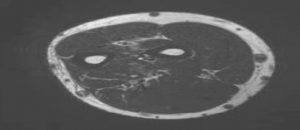
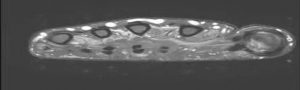
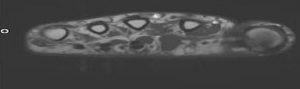
Patient underwent MRI of the right upper extremity with representative images as followed.
What is the next step?
 |
 |
 |
 |
Answer:
3) MRI of the cervical spine
Question:
Patient’s neurologist calls you to discuss the findings.
Which one is the most likely etiology in your opinion?
 |
 |
Answer:
4) Myelomalacia and atrophy
Question:
Neurologist mentions that patient had a recent brain MRI that was normal.
Neurologist also thinks that the extent of right upper extremity weakness and atrophy is out of proportion to the degenerative disc disease at this level.
As a radiologist, what do you recommend as the next step?
Answer:
3) Cervical spine MRI with flexed neck
Question:
Now, according to the cervical MRI in flexion position, what is your diagnosis?
 |
 |
Answer:
4) Non progressive juvenile spinal muscular atrophy (Hirayama disease) with motor neuropathy and muscles denervation.
Findings:
- Axial PD and PD fat sat images of the right forearm and hand demonstrate denervation changes and fatty atrophy of the muscles.
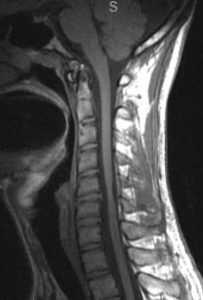
- Sagittal T1 and T2 magnetic resonance imaging (MRI) of Cervical spine in neutral position show straightening of cervical spine with segmental cord atrophy and intramedullary hyper intensity at C5–C6 level; note the “sand watch” appearance in neutral position with normal cord architecture above and below the atrophy. The dura is in a normal position.
- MRI in flexion position shows anterior displacement of the dorsal dura compressing the thecal sac, with a prominent dorsal epidural compartment and flow voids seen in the posterior epidural space.
Discussion:
- Non progressive juvenile spinal muscular atrophy, also known as Hirayama disease, is characterized by the insidious onset of unilateral or asymmetric oblique amyotrophy that affects the C7, C8 and T1 myotomes.
- It typically occurs mainly in young males between the ages of 15-25 years and is characteristically associated with cold paresis.
- The onset is insidious, and is characterized by muscle weakness and atrophy in the hand and forearm, with sparing of the brachioradialis without sensory or pyramidal signs, giving the characteristic appearance of oblique amyotrophy.
- The amyotrophy is unilateral in most patients, asymmetrically bilateral in some and rarely symmetric. Hirayama disease is a benign, non progressive motor neuron disease.
- Chronic microcirculatory changes in the territory of the anterior spinal artery induced by repeated or sustained flexion account for the necrosis of the anterior horns of the lower cervical cord, which is the hallmark on pathology.
- Magnetic resonance imaging in neutral position shows focal areas of cord atrophy in the lower cervical and cervico-dorsal junction as asymmetric flattening of cord with areas of gliosis appearing hyper intense on T2W images.
- MRI in flexion position reveals, anterior displacement of the detached posterior dura from the underlying lamina compressing the thecal sac, widened posterior epidural space seen as crescentic area or epidural mass of signal alteration appearing with flow voids within.On post contrast images, uniform enhancement of this crescentic area is noted. These flow voids were likely the engorged posterior venous plexus as they got completely effaced with acquiring the scan again in a neutral position.
Gupta K, Sood S, Modi J, Gupta R. Imaging in Hirayama disease. J Neurosci Rural Pract. 2016 Jan-Mar;7(1):164-7.
Raval M, Kumari R, Dung AA, Guglani B, Gupta N, Gupta R. MRI findings in Hirayama disease. Indian J Radiol Imaging. 2010 Nov;20(4):245-9.
Courtesy of Parham Pezeshk,MD, Assistant Professor, Division of Musculoskeletal Imaging Department of Radiology, University of Texas Southwestern Medical Center,Dallas,TX
